 Surgery for the thyroid gland is now undergoing a significant advance. thanks for minimally invasive surgery.
Surgery for the thyroid gland is now undergoing a significant advance. thanks for minimally invasive surgery.
Traditional, conventional surgery of the thyroid gland uses a standard, open-surgery approach requiring an incision that is four to five inches in length. The result is a noticeable and sometimes prominent, life-long scar on the lower portion of the patient's neck.
A minimally invasive approach to thyroid surgery requires an incision that is only an inch or less in length. Through this small
hole, the surgeon inserts a tiny endoscope that is only a half-centimeter in diameter. This instrument permits he/she to see the
thyroid gland and surrounding tissue without having to physically expose it. With the scope, the surgeon can view the gland on a video monitor. They can then remove (resect) portions of thyroid tissue. This scalpel uses ultrasonic energy to gently and precisely cut tissue and to seal off (ligate) blood vessels, significantly reducing operative time in thyroid surgery.
To date, only a few centers in the U.S. have committed to the training and equipment required for performing this superior procedure.
While many patients today are candidates for minimally invasive endoscopic surgery, a significant percentage has a gland too large to remove through a small opening. In these cases, the surgeon must use tradition methods to remove the thyroid. This approach is a safe, and long-used and established, operation. It is an important part of an endocrine-surgery group's options, especially for patients with large goiters, inflammatory conditions, and hyperthyroidism.
Surgical Treatment
Conventionally, patients received general anesthesia for thyroid surgery, although some patients may only need local anesthesia and moderate sedation for thyroidectomy. Thyroid surgery normally takes between 30 and 90 minutes, depending on whether the surgeon removes the entire gland.
Minimally invasive surgery is typically an outpatient procedure, with most patients going home within in a few hours of the operation. Traditional surgery almost always means at least a one-night stay in the hospital.
Any patients undergoing thyroid surgery will experience a few days of hoarseness and soreness in the throat, but patients who undergo the minimally invasive procedure will have less discomfort around the external wound. This helps to speed recovery. Patients can usually go home the same day as their minimally invasive surgical procedure and resume most normal activities the next day.
Full or Partial Thyroidectomy
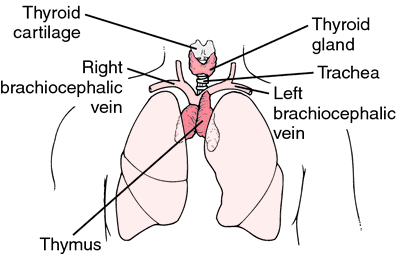
The thyroid is a butterfly-shaped gland at the front of the neck. An undiagnosed thyroid nodule is the most common condition for which patients undergo thyroid surgery. Most patients with thyroid growths are candidates for the minimally invasive approach; however, conducting a thorough and conclusive evaluation is often difficult with thyroid lesions, unless the growth or the gland itself is completely removed. Therefore, the biopsy is performed after some portion of thyroid removal.
Roughly half of thyroid surgery patients receive a total removal of the gland (thyroidectomy), while the other half of this population will only undergo removal of the left or right side of the gland (lobectomy). Patients with a known cancer of the thyroid will receive a complete thyroidectomy. For patients receiving a partial removal, a portion of the gland must undergo pathology analysis in the lab to assure that is it safe to leave the remaining portion of the gland behind. In partial thyroidectomy, the team sends the removed portion of the gland for immediate evaluation by a pathologist while the operation is going on. Based on this analysis the surgeon may remove the remaining portion of the gland or leave it in place. The pathologist further evaluates the removed sample after the surgery is complete. Based on this analysis, a second surgery is necessary in a few cases.
High Satisfaction and Preference for Minimally Invasive Surgery
The level of satisfaction about the experience of undergoing minimally invasive thyroid surgery, and about the outcomes from it, has been very high among patients and medical professionals (including referring endocrinologists and family physicians). Many more patients could be benefiting from this capability if awareness of its availability was higher among patients and the medical community. Aria was the among the first centers in the region to offer minimally invasive thyroid surgery.
Making the care determinations described above and offering the right, best, and most advanced treatment for thyroid disorders, requires a specialty group with significant experience and training, and a dedicated focus on thyroid care. Aria's thyroid service is provided by a team with exactly this type of commitment.